The brachial plexus is a set of nerves that connects your neck to your arm. It includes five primary nerves, each serving different parts of the arm. The brachial plexus controls movement and sensation in the arm. Brachial plexus injuries in adults often occur as a result of serious car accidents or blunt trauma.
In infants, brachial plexus injuries are often a result of the delivery process. Most babies fully recover in 3 to 9 months, but some experience serious health problems. (R)
While brachial plexus injuries are often referred to as “Erb’s palsy,” Erb’s palsy refers to a specific subset of brachial plexus injuries. Erb’s palsy affects the top brachial plexus nerves and typically affects the upper arm but not the hand and fingers. Brachial plexus injuries that affect only the hand are called “Klumpke paralysis.” Brachial plexus injuries may affect just the upper part of the arm as in Erb’s palsy, just the hand as in Klumpke paralysis, or the entire arm. (R)
This page will review the types of brachial plexus injuries, causes of Erb’s palsy, symptoms, treatment, and ways to seek a legal claim if your child’s brachial plexus injury was caused by negligence or a medical error.
Contents
- Brachial Plexus Injuries and Erb’s Palsy: What You Need to Know
- How can the brachial plexus be damaged?
- What are the symptoms of a brachial plexus injury?
- What types of treatment are available for brachial plexus injuries?
- What are the legal issues surrounding brachial plexus injuries?
- What questions should I ask my doctor?
- What should I expect if my child has a brachial plexus injury?
How can the brachial plexus be damaged?
The brachial plexus may be damaged in a number of different ways. Damage is categorized by the effect on the nerve itself and by the location of the injury.
- Neuropraxia: The nerve is stretched or compressed but are not torn. Neuropraxia generally heals on its own within a few months. (R)
- Neuroma: The nerve is stretched and damaged, leaving scar tissue behind. The nerve will mostly heal on its own, but some damage may remain. (R)
- Rupture: The nerve is stretched and tears, but the tear is not at the spinal cord. A rupture will not heal without intervention. In some cases, a donor nerve graft may be used to partially repair the rupture. (R)
- Avulsion: the nerve is torn away from the spinal cord. This damage is permanent and irreparable. (R)
Causes of Erb’s Palsy
Brachial plexus injuries occur when the baby’s head and shoulders are stretched too far during delivery. This type of stress usually occurs because the delivery is particularly difficult. In some cases, brachial plexus injuries may be the result of ordinary contractions. Babies with underdeveloped neck and shoulder muscles are also at risk for brachial plexus injuries even in relatively easy deliveries.
Difficult Deliveries
Factors that increase the difficulty of delivery and the likelihood of a brachial plexus injury include large infant size, or “fetal macrosomia,” and breech presentation. (R)

Babies of average size are already a tight fit in the birth canal and babies with fetal macrosomia are even more difficult. The baby cannot stay in the birth canal for an extended period of time because the pressure limits the baby’s supply of oxygen, potentially causing a range of serious side effects. To avoid those problems, doctors want to get the baby out of the birth canal in a timely manner. So, your doctor may attempt to pull the baby through the birth canal by the head or by the arms.
The force exerted on the baby’s arms and shoulders may damage the baby’s brachial plexus. The risk is increased by use of equipment such as vacuum extraction tools or forceps to move the baby out of the birth canal. With or without the aid of doctor, large babies’ heads may be pulled to the side during delivery as their shoulders are forced through the narrow birth canal, stretching the brachial plexus.
A breech presentation also increases the risk of brachial plexus injuries. Ideally, babies are born head first and with their arms to their sides. This creates the most streamlined shape to pass through the birth canal. In a breech presentation, the baby is born feet-first. That means the baby’s arms are stretched over its head during the delivery, potentially stretching and damaging the brachial plexus. About 40% of brachial plexus injuries may require surgery. (R)
Delivery may involve a wide variety of complications, including changes to the mother’s or baby’s heart rate and blood pressure. Depending on the circumstances, a delivery complication may require speeding up the process so that the baby or the mother can receive treatment. That means the doctor may need to exert some force to pull the baby through the birth canal, increasing the risk of brachial plexus injury.
See also: Preeclampsia: High Blood Pressure and Your Baby
Contractions
Brachial plexus injuries can happen as a result of strong contractions during the delivery process. During a contraction, powerful muscles squeeze down on the uterus to force the baby out toward the birth canal. That pressure may damage the baby’s brachial plexus.
Underdeveloped Neck and Shoulder Muscles
Babies may have underdeveloped neck and shoulder muscles for a number of reasons, including premature birth, congenital issues, and more. Babies with weak or underdeveloped neck and shoulder muscles are especially likely to suffer brachial plexus injuries during delivery.
See also: Why Pregnant Women Should Consider Taking Folic Acid
What are the symptoms of a brachial plexus injury?
Mild brachial plexus injuries may cause numbness or tingling in all or part of the arm. It may be difficult to identify a mild brachial plexus injury in a newborn because they can’t tell you what they’re feeling.
Mild brachial plexus injuries can also cause weakness of the arm. Your doctor may be able to detect that weakness using the Apgar test administered to all babies after birth. Among other things, the Apgar test involves checking muscle tone. Weak muscle tone in one arm may indicate a brachial plexus injury. Your doctor may also be able to detect a brachial plexus injury with a Moro test. This is a standard test performed on all newborns to test the “Moro reflex.” It involves simulating a falling sensation to check whether the baby is startled and flexes its arms and hands in response. If the baby has no Moro reflex, a brachial plexus injury may be at fault. (R)
More severe brachial plexus injuries will have more obvious symptoms. Brachial plexus injuries may prevent the baby from moving the affected arm and may cause a weakened grip in that hand. In some cases, the baby’s arm will turn inward and the elbow will flex, holding the arm against the baby’s body.
Your doctor may take x-rays of your baby’s shoulders to rule out the possibility of broken bones, which may cause similar symptoms. Your doctor may also use an electromyogram (EMG) to measure muscle damage related to the injury or perform a nerve conduction study (NCS) to measure the damage to the brachial plexus nerves.
Some types of nerve damage are painful. Your baby can’t tell you what hurts, so you’ll need to be alert to signs that your baby isn’t moving one arm or cries when that arm or shoulder is disturbed, as these may be signs of a brachial plexus injury.
Conditions Caused by Brachial Plexus Injury
The brachial plexus includes several different nerves. Brachial plexus injuries are categorized by which nerves and parts of the arm are affected. Different types of brachial plexus injuries cause different conditions with distinct symptoms. Conditions caused by brachial plexus injuries include global palsy, Klumpke’s palsy, and Erb’s palsy.
The symptoms and outcomes associated with each condition depend on the severity of the brachial plexus injury. The most serious types of damage are avulsion, where the nerves are torn from the spinal cord, and rupture, where the nerves are torn in a different area. This type of damage is typically irreversible. A neuroma is less severe and occurs where the nerve is compressed or scarred and can’t send signals efficiently. The least severe type of damage is a neuropraxia, which occurs when the nerve is stretched or compressed but not torn. Neuropraxias are often treatable and may even heal entirely.
Global Palsy
Global palsy is caused by an injury to all five nerves of the brachial plexus. A child with global palsy will have no ability to move the affected arm or hand and may or may not have sensation in the affected arm. (R)
Klumpke’s Palsy
Klumpke’s palsy (also known as Dejerine-Klumpke palsy or Klumpke’s paralysis) occurs as a result of damage to the eighth cervical (C8) and first thoracic (T1) nerves. These nerves control the hand, wrist, and forearm. Klumpke’s palsy may cause your baby’s hand to curl up into a claw. It may cause loss of feeling and weakness in the hand and lower arm. (R)
Erb’s Palsy
Erb’s palsy (also known as Erb-Duchenne palsy) is caused by damage to the fifth and sixth cervical (C5 and C6) nerves. These nerves control the upper arm and shoulder. Erb’s palsy may cause your child’s arm to curl up against the body and turn inward in a pose called “waiter’s tip.” Depending on the severity of the damage, Erb’s palsy may stunt the growth of the affected arm and cause circulatory problems. Erb’s palsy may also cause a loss of sensation in the arm. (R)
What Doctors Look for in a Brachial Plexus Injury
Brachial plexus injuries may range from minor damage that clears up in a few months to major injuries with lifelong consequences. Your doctor will do basic muscle and reflex tests shortly after your baby is born and may detect signs of a brachial plexus injury at that point. However, not all injuries are readily diagnosable so early.
If you notice that your child isn’t moving one arm, has a weak grip with one hand, or is holding an arm in an unusual position, contact your doctor to ask whether your child may have a brachial plexus injury. You should also be alert for crying and other behavior that may indicate that your baby is in pain. Brachial plexus injuries may be treatable with surgery and physical therapy, so it’s important to act fast if you believe your baby may have suffered damage to the brachial plexus nerves. (R)
See also: Cerebral Palsy: What You Need to Know
What types of treatment are available for brachial plexus injuries?
Brachial plexus injuries occur when the brachial plexus nerves are stretched, compressed, torn, or ripped away from their connection to the spinal cord. The brachial plexus nerves connect the arm and hand to the brain, so brachial plexus injuries affect arm and hand function. Treatment for brachial plexus injuries depends on the type and severity of the injury.
Neuropraxia Treatment
Neuropraxia is the least severe type of damage to the brachial plexus nerves. It refers to stretching or compression of the nerves without tearing or rupture. These types of nerve injuries will often heal on their own or with modest physical therapy. The damaged portions of the nerves will regrow over time from the neck down at a rate of about 1 inch per month. If your baby’s nerves are healing well, you’ll typically see the elbow start to bend within about 3 months. Movement of the fingers and wrist are also good signs. (R)
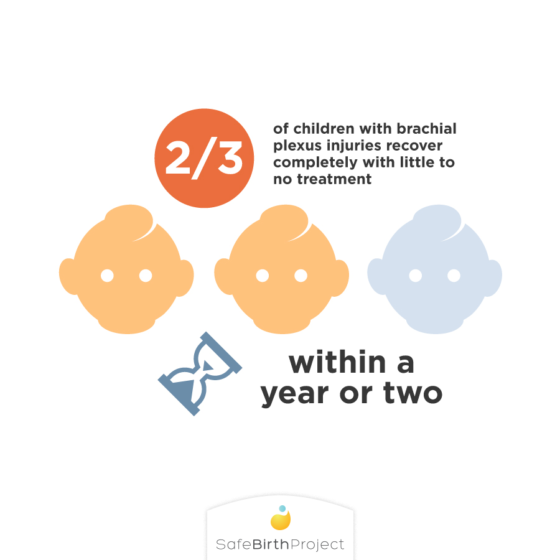
About two-thirds of babies with a brachial plexus injury will recover fully with minimal treatment or no treatment at all. Incomplete recovery is typically only visible once children become older. (R)
Surgical Intervention
Very severe neuropraxias and other types of nerve injury will not heal on their own and may require surgery. Surgery to repair damaged nerves must be done within a relatively short time-frame after the original injury. Otherwise, the muscles in your baby’s arm will weaken too much and the nerves won’t reattach to them. These surgeries may be performed as early as 3 months after birth for severe injuries. (R)
Surgery is always risky, especially for newborns. Your doctor will perform a range of tests to determine if your baby is a good candidate for surgery. Surgery will not give your baby perfect use of the arm, but can offer some improvement. If the injury is less severe, you and your doctor may decide to wait for a few months to see how much the injury improves on its own. More severe injuries may require earlier surgical treatment.
Because babies can’t talk about their symptoms and don’t have the coordination to perform tests of nerve and muscle function, the surgeon may not be able to judge what type of surgery will be needed or even what type of damage your baby has suffered until she can actually look at the nerves. Your surgeon will give you her best guess as to what to expect, but the plan may change depending on the type of damage she finds and what will be required to fix it.
The type of surgery needed to repair a brachial plexus injury depends on the type of damage your baby’s nerves have sustained.
Neuroma Surgery
Neuroma refers to a buildup of scar tissue on a nerve that compresses and damages the nerve. Surgery to repair a neuroma depends on the severity of the damage. A “neurolysis” procedure may be required to remove the scar tissue surrounding a nerve, relieving the pressure on the nerve and allowing it to heal on its own. If the neuroma is larger and more severe, a “neuroma excision” may be required. A neuroma excision is a procedure in which the surgeon removes the section of the nerve surrounded by scar tissue. The undamaged nerves on either side of the section that was removed may be long enough to connect directly. Otherwise, the surgeon will use a nerve graft to bridge the gap between the two ends. (R)
A “nerve graft” is a procedure in which the surgeon takes healthy nerves from somewhere else in the body and uses them to fill in the gap between damaged nerves. Hand function, for example, is impaired in about 15% of cases. The grafts provide a guide that shows the damaged nerves where to grow as they heal. In infants, the nerves used in the graft are typically taken from the baby’s calf or heel. A small part of the calf or heel may lose some sensation, but should have full movement. (R) (R)
Rupture and Avulsion
Rupture refers to the tearing of a nerve somewhere along its length. Avulsion refers to the tearing of the nerve from its connection to the spinal cord. These are very serious injuries and can have a major impact on the function of your child’s arm. Ruptures and avulsions may require nerve grafts to reconnect the nerve where it has torn. If the damage is very severe, your surgeon may need to use donor nerves in place of or in addition to nerves taken from your baby’s leg. (R)
In some cases, brachial plexus injuries may be treated with a “nerve transfer.” Where a nerve graft simply acts as a path along which the damaged nerves can regrow, a nerve transfer actually replaces the damaged nerves. Your surgeon will take an undamaged nerve from a nearby part of the body and connect it to the muscles that were served by the damaged nerve. This can restore some sensation and movement to the affected muscles. The muscles that were originally controlled by the undamaged nerve will lose function, but other nearby muscles will typically take up the slack to make up for that loss.
Muscle Transfers
Brachial plexus injuries may not heal evenly, causing imbalance and weakness as certain muscle groups recover better than others. If that imbalance is severe, your child may need a muscle transfer procedure. In a muscle transfer procedure, your surgeon will move stronger muscles and tendons into place to support weaker ones. (R)
Other Treatments: Physical Therapy, Botox
Your baby may benefit from physical therapy to improve flexibility and range of motion in the affected arm. Physical therapy is particularly important if your child has had surgical treatment for a brachial plexus injury. Physical therapy, like motion exercises, can improve blood flow and muscle tone to promote healing and avoid side effects such as muscle cramps and joint stiffness. (R)
Brachial plexus injuries may cause one group of muscles to be too weak to fully exercise a joint. For example, your child may not be able to fully straighten the elbow. If you don’t use the full range of motion in your joints, you start to lose it. If your child can’t fully exercise a joint, your doctor may recommend the use of a splint to hold the arm in the proper position. The splints will be periodically upgraded as your child grows and develops. Splints may be used in conjunction with physical therapy and after surgery.
Some brachial plexus injuries may cause a group of muscles to tense up and pull a joint into the wrong position. If this tension is very strong, your child may need an injection of botulinum toxim (Botox) to relax those tense muscles and allow the joint to return to its natural position. With Botox relaxing the very tense muscles, correcting imbalance, your child will be able to exercise and strengthen weaker muscles and use the full range of motion of the affected joints. (R)
Recovery Expectations
As mentioned above, about 65% of children with brachial plexus injuries will recover completely with little to no treatment. These cases typically clear up within a year or two and won’t require any followup. (R)
If your child needed surgery to repair a brachial plexus injury, recovery may take longer. Most of the healing and recovery will still happen within the first year, but improvement will continue for several years. Your child will likely need regular physical therapy for a couple of years to ensure that the arm is developing properly. The arm affected by the brachial plexus injury may not develop like the unaffected arm — it may be smaller, shorter, and weaker. Regular physical therapy can improve the functionality of the affected arm, but children with injuries severe enough to require surgery typically do not regain full function.
What are the legal issues surrounding brachial plexus injuries?
Injuries to the brachial plexus, the bundle of nerves that control the arm and hand, are typically caused by trauma. In adults, car accidents and sports injuries are common causes. In infants, brachial plexus injuries are often cause by birth-related trauma.
In some cases, a brachial plexus injury may be caused by a very strong contraction. In other cases, brachial plexus injuries may occur when the baby gets lodged in an unusual position in the womb or in the birth canal. These injuries are generally unavoidable.
Unfortunately, many brachial plexus injuries are caused by the actions of doctors and other medical care staff during delivery. When the negligence of a doctor or other medical care provider causes your child’s injury, you and your child may be entitled to compensation for the damage.e”]
Proving Medical Malpractice and Negligence
The basis for a medical malpractice lawsuit (a suit against a medical care provider) is typically negligence. That’s a legal term that means the doctor, nurse, or other medical staff did not meet the accepted standard of care in treating your child. The exact method of determining the standard of care varies from state to state, but usually involves testimony from other doctors who work in the same field about what the best practices are and why your care provider’s actions did not meet that standard.
In order to win compensation, you’ll need to prove several elements. First, your doctor or other relevant hospital staff must have had a duty to you and your child. This may be called a “doctor-patient relationship.” The medical care team creates a doctor-patient relationship when they start treating you, so this element is usually easy to prove.
Next, you’ll need to show that your child was injured. In the case of a brachial plexus injury, that may involve showing medical records for the treatment your child needs. It may also involve testimony from doctors and other medical care staff that have treated your child for the injuries in question.
Third, you’ll need to show that the doctor or other care provider acted negligently. As mentioned above, that will involve having other medical experts testify about what the appropriate standard of care is. Finally, you’ll need to show that the care provider’s negligence caused your child’s injury. This is called “causation” and is often one of the most difficult elements of the case. If your doctor acted negligently but didn’t cause injury to your child, you don’t have a case. If your doctor acted negligently but your child’s injury was caused by something else, you don’t have a case. You have to show a clear link between the negligence and the injury.
Causation in Brachial Plexus Injury Cases
Brachial plexus injuries are often caused by trauma during delivery. Brachial plexus injuries occur when the baby’s head is pushed to the side or when too much pressure is put on the baby’s arms or shoulders during delivery. That can happen when the baby is large and can’t pass through the birth canal easily or when the baby is born feet-first (breech). The baby can’t stay in the birth canal for too long because of the risk of oxygen deprivation, so your doctor may pull on the baby or use forceps or vacuum suction to get the baby out. Pulling on the baby may strain the baby’s neck and shoulders and cause brachial plexus injury.
Doctors and nurses are trained to deliver a baby as safely as possible, but they may pull too roughly or in the wrong direction during the stress of a difficult delivery. In addition, a doctor or other medical care provider may fail to realize that the baby’s shoulders are stuck in the birth canal and attempt to pull the baby out instead of performing an emergency cesarean section.
To prove causation in a brachial plexus injury case, you’ll show that your doctor pulled on the baby’s head, shoulders, or legs or used forceps or vacuum suction to speed up delivery. You’ll then show that your child suffered a brachial plexus injury and that the doctor’s actions were likely the cause.
Compensation for Brachial Plexus Injuries
If your child is injured by medical negligence, your family may be entitled to two different types of compensation: economic and non-economic. Economic compensation refers to monetary losses caused by the injury. That may include past and future medical expenses. It may also include lost income for your child — income that your child could have earned without the injury. Non-economic damages refer to losses that aren’t monetary, such as the pain and suffering your child experienced as a result of the injury. In rare cases, you may also be entitled to damages for “loss of consortium,” or loss of time and enjoyment with your child due to the injury.
Many medical negligence cases never go to trial. Instead, they are settled before a trial happens. Your attorney will help you negotiate any settlement offer to make sure you’re getting fair treatment. If your case is very strong, the settlement offer will be similar to what you would receive if you won at trial. If your case is weaker, you may be offered less than that amount. You’ll need to discuss your options with your attorney and your family to decide whether to accept a settlement. If you accept, you will give up the right to sue for more money. If you don’t, you’ll be stuck with the decision of the jury at the trial or on appeal.
When to Speak to a Birth Injury Attorney
If you believe that your child suffered a brachial plexus injury as a result of medical negligence, you should speak to an experienced local attorney as soon as possible. The law limits the amount of time you have to file a lawsuit, so act quickly. Your attorney can help you gather the medical evidence you need and will find the necessary expert witnesses to testify about the standard of care you and your child should have received.
Reputable law firms generally offer a free consultation and case evaluation, so you can speak to an experienced attorney about your case without paying anything at all. You can hear a reliable opinion about your case and you can visit multiple firms to find a lawyer you trust. In addition, most law firms take medical malpractice cases on a contingent-fee basis. That means their fee is a percentage of your damage award. If you don’t win anything, you don’t pay anything. Remember to ask about the fee structure of any law firm you consult about a potential medical malpractice case.
If you need legal help, consider contacting Safe Birth Project for more information.
What questions should I ask my doctor?
The brachial plexus is a group of nerves that runs from the neck and shoulder through the arm. Damage to the brachial plexus affects the function and sensation of the arm.
So, what do you need to know about your child’s brachial plexus injury? Here are some common questions you should ask your doctor.
1. What can I do to minimize the damage?
Most brachial plexus injuries are minor and will heal on their own. Your doctor may be able to give you gentle stretching exercises to do with your baby to promote proper healing of the nerves.
2. Will my child need surgery?
While mild brachial plexus injuries typically heal within a few weeks, more serious cases require surgical intervention. Ask your doctor what you should be watching for when you take your new little one home. What are the signs that the nerves aren’t healing properly?
Surgeries to repair brachial plexus injuries must be performed fairly early, before the arm muscles degrade too much to repair. Ask your doctor about the time frame for the surgery so you have time to prepare.
3. Will my child need physical therapy?
Physical therapy can help maintain strength and flexibility in the affected arm. Ask your doctor about whether physical therapy is right for your child and ask for a list of qualified physical therapists.
4. What is my child’s long-term outlook?
Severe brachial plexus injuries can permanently impair your child’s ability to use the affected arm. That means your little one may need occupational therapy to learn how to do everyday tasks with one arm.
Remember, every child is unique and your doctor will be able to give you advice tailored to your child’s needs. Don’t be afraid to ask questions until you’re confident that you understand your child’s injury and needs.
What should I expect if my child has a brachial plexus injury?
Your new little one has been diagnosed with a brachial plexus injury. Whether it’s a general brachial palsy, Klumpke’s palsy, or Erb’s palsy, you’re probably wondering what to expect. Let’s review.
Diagnosis
As soon as you deliver, your doctor will perform a standard Apgar test on your baby. It involves checking your baby’s heart rate, reflexes, breathing, and muscle tone to make sure your baby is healthy. Doctors are looking out for labored breathing, high or low heart rate, and weakness of the muscles. If your baby has weak arm or hand muscles on one side, your doctor may want to perform further tests to check for a brachial plexus injury.
These tests may include checking for a “Moro reflex” or looking at the baby’s shoulder with an MRI to check for nerve damage. Your doctor may want an x-ray of the baby’s shoulder and arm to check for broken bones, which can have similar symptoms as a brachial plexus injury but require immediate treatment.
In some cases, a brachial plexus injury won’t be easily diagnosable right away. It may take time for symptoms to become evident. Once you’ve taken your baby home, you may notice that the baby’s arm is weak or turned inward or that the baby can’t move the arm at all. If you notice these symptoms, you should schedule an appointment with your doctor right away to check for brachial plexus injuries. Your doctor will use the same tests described above to determine whether a brachial plexus injury is the cause of your little one’s symptoms.
You may be given a specific diagnosis such as Erb’s palsy or Klumpke’s palsy. These names refer to different types of brachial plexus injuries. Erb’s palsy typically affects the upper arm and Klumpke’s palsy typically affects the forearm and hand.
Treatment
Once you have a diagnosis, treatment depends on the severity of the injury. About two-thirds of cases will recover completely with minimal treatment. Your doctor may give you a set of gentle exercises to do with your baby to help strengthen the arm muscles and improve flexibility in the joints. If the injury is healing properly, the baby will probably start to bend and straighten the elbow by around 3 months of age. Shortly after that, you should see movement in the hand and wrist.
You will visit with your doctor regularly for checkups on your child’s progress and you’ll likely need to continue the exercises for several months. Most children will completely recover by their first birthday, although you may see some improvement into their second year.
Surgery
If the injury is too severe to heal on its own, your child may need surgery to repair the damaged nerve. The timing of this type of surgery is crucial. You have to wait long enough to see if the injury will heal on its own. If you wait too long, however, the muscles may weaken so much that surgery becomes impossible. You’ll need to work with your baby’s care team to track the healing process and decide if and when surgery is the best option.
Several different types of surgery may be required to repair a brachial plexus injury. In some cases, it may be enough to remove the scar tissue around a damaged nerve or to remove the damaged portion of the nerve. In other cases, a nerve graft or transfer, such as a tendon transfer, may be required. (R)
If your baby needs surgery, you can expect a hospital stay of a few days to a week. After that, you’ll work with your baby’s surgeon and physical therapist to develop a treatment plan. In some cases, your surgeon may recommend a splint to hold your baby’s arm in the proper position for a few months after surgery. You may be given exercises to do with your baby at home or you may have regular appointments with a physical therapist.
Long-Term Recovery
Most children with brachial plexus injuries recover completely; however, children with injuries severe enough to require surgery will likely not have perfect use of the affected arm. Surgery may restore some function and sensation but cannot offer a perfect fix. The arm may be stunted due to poor circulation and it will be weaker than the unaffected arm. If the damage was particularly severe, your child may never have use of the affected arm.
Your child may need ongoing physical therapy to strengthen the arm and maintain joint flexibility. If use of the arm is extremely limited, a physical therapist can teach your child strategies for completing everyday tasks with limited or no use of one arm.
Finally, you’ll need to keep a close eye on the affected arm. That arm will often have limited sensation and restricted circulation, so your child may not notice an injury right away and the injury may take a long time to heal. For the same reason, you’ll need to take extra care to keep the affected arm warm when the weather gets cool.
It’s never going to be easy to see your child injured, but brachial plexus injuries are rarely serious. With some physical therapy and lots of love and support, even a severe brachial plexus injury won’t hold your child back.
Brachial Plexus Injuries and Erb’s Palsy Resources for Parents
Like any injury, brachial plexus injuries can come with big medical bills. In addition, your child may never have full use of the affected arm. These resources are designed to help children with disabilities and their families.
- Medicare and Medicaid: Medicare and Medicaid can cover your child’s medical costs, including any necessary surgeries.
- Social Security disability benefits: Your child may be entitled to Social Security disability benefits, which can help ease the financial burden of medical bills and other necessary expenses.
- United Brachial Plexus Network: The United Brachial Plexus Network (UBPN) provides support for children with brachial plexus injuries. UBPN gives access to medical devices and educational materials focused on brachial plexus injuries.
- Online communities: Search online for websites and blogs dedicated to children with brachial plexus injuries such as Erb’s palsy. These online communities can provide emotional and sometimes financial support for children with brachial plexus injuries and their parents.
